Abstract
Background
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, complement-mediated hemolytic anemia caused by a somatic phosphatidylinositol glycan class A (PIGA) gene mutation on the X chromosome of hematopoietic stem cells. The mutation of PIGA gene destroys the biosynthesis of glycosylphosphatidylinositol (GPI), resulting in the lack of GPI anchor proteins, including CD55 and CD59 molecules, in hematopoietic stem cells and their progeny cells (erythrocytes, granulocytes, monocytes, lymphocytes). Erythrocyte membrane without CD55 and CD59 are prone to complement attack and lysis[1]. PNH presents as hemolytic anemia, bone marrow failure, and thrombosis, and so on. Targeting the terminal complement inhibitor, such as eculizumab (C5 inhibitors), could not only control hemolytic anemia, reduce thrombosis and transfusion, improve the staging status of chronic kidney disease, and prevents the deterioration of renal function in PNH patients. However, eculizumab has not yet been available in mainland of China, glucocorticoids is still used as the first-line therapy in China.
Methods
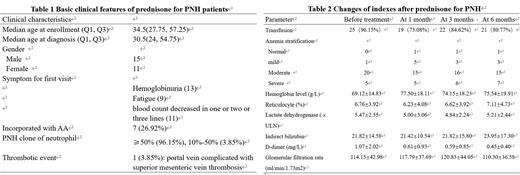
From September 2020 to April 2022, 26 PNH patients with high disease activity (HAD) were enrolled in the study. Oral prednisone was initiated at a dose of 1mg/kg/day and gradually tapered four weeks later. Clinical characteristics of patients was described in Table 1.
Results
The hemoglobin paired T-test results before treatment and at 1 month, 3 months, and 6 months after treatment were as follows: (69.12±14.83) vs (77.50±18.11), p<0.05;(69.12±14.83) vs (74.15±18.23), p=0.15;(69.12±14.83) vs (75.54±19.91), p=0.09; paired chi-square test (McNemar Test) for anemia stratification (>90g/L, 60-90g/L, <60g/L) showed no marked changes: p=0.082, p=0.344, p=0.247; By Friedman Test, it showed reticulocyte percentage was also similar: (6.76±3.92) vs (6.23±4.08) vs (6.62±3.92) vs (7.11±4.73), p=0.457.
Before treatment, 25 patients (25/26, 96.15%) were transfusion dependent. After treatment at 1 month, 3 months, 6 months, 19 patients (19/26, 73.08%), 22 patients (22/26, 84.62%), 21 patients (21/26, 80.77%) were transfusion dependent, respectively (p=0.031; p=0.375; p=0.219). Two patients progressed to transfusion dependent at 3 months, 6months, respectively.
No patients achieved remission of hemolysis (LDH < 1.5 ⅹULN) at 1, 3, and 6 months; the level of lactate dehydrogenase and indirect bilirubin (IBIL) showed no changes by analysis with Friedman test (p=0.436, p=0.881).
By Friedman test, the serum level of D-dimer also showed no changes at different times ( p=0.263). Level of D-dimer elevated (>0.55mg/L) in seven patients before treatment, and returned back within normal range in one patient at 1 month, two patients at 3 months, three patients at 6 months. But among the people with normal D level initially, one patient and three patients each had elevated D-dimer level at 3 months and 6 months, respectively.
Two patients achieved renal function improvement at 3 months, 6months, respectively. But three patients had renal function deterioration after treatment. Glomerular filtration rate (GFR) was (114.15±42.98) ml/min/1.73m2 before treatment, and become (117.79±37.69) ml/min/1.73m2, (120.85±44.05) ml/min/1.73m2, (110.30±36.58) ml/min/1.73m2 at 1, 3, and 6 months (p=0.42, p=0.43, p=0.41).
Discussion
Previous studies have mainly compared the improvement of anemia after breakthrough of PNH by glucocorticoids therapy. The improvement of anemia could not be ruled out as a result of transfusion support or the reduction of temporary hemolysis after breakthrough of PNH. We found the level of LDH increased along with improvement of hemoglobin during prednisone treatment, and percentage of reticulocytes was not changed at same time. It suggested that the improvement of anemia in some patients may not be caused by controlling intravascular hemolysis or the compensatory hyperplasia of the bone marrow, but by transfusion.
Conclusions
It preliminarily showed prednisone maintenance therapy for PNH could not control hemolysis and thrombosis, and could not improve anemia and renal function. The efficacy of glucocorticoid maintenance therapy in PNH is uncertain.
Reference:
[1] Brodsky R A. How I Treat Paroxysmal Nocturnal Hemoglobinuria[J]. Blood, 2021, 137(10): 1304-1309.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal